Research
The Center for Health Disparities strives to develop an integrated, thematic research agenda focused on the genomic and physiological mediators (and impacts) of the social determinants of health disparities (encompassing genetics, epigenetics, health behaviors, “big data” analytics, physical and social environments, and environmental exposures).
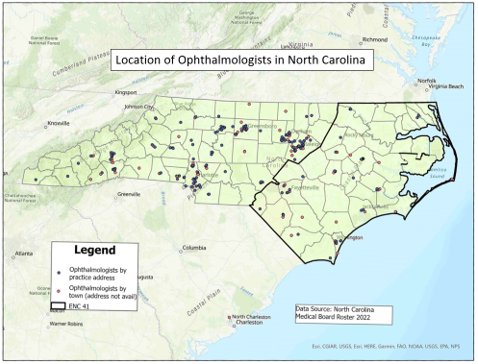
Accessing the Ophthalmology Landscape of North Carolina
ECU Investigators: Dr. Jessica Cooke Bailey, Dr. Katherine Jones
Dr. Cooke Bailey’s research focuses on vision health disparities, and as she is new to East Carolina University, this study, in collaboration with Dr. Katherine Jones, will seek to better understand the ophthalmology and optometry needs of the state of North Carolina, with particular focus on the Eastern region. This will serve as a jumping-off point to expand All Eyes on Us (described below) to North Carolina, as better understanding access to vision care will illuminate potential points of intervention.
Jamaica Eyes
ECU Investigator: Dr. Jessica Cooke Bailey
This study investigates the prevalence and severity of glaucoma in Afro-Caribbean populations by partnering with clinical PI, Ophthalmologist Dr. Camara Brown at Kingston Public Hospital (KPH) in Jamaica. Co-led by Drs. Cooke Baley and Brown, along with Briana McIntosh of Case Western Reserve University (CWRU), the team created standard operating procedures for obtaining research-quality data from clinical charts and analyzed clinical data collected at KPH during site visits to characterize the clinical profile of Jamaican glaucoma. The findings present the first-ever summary of optic nerve head (ONH) parameters of glaucomatous eyes from Jamaican adults, which can form the clinical baseline of glaucomatous eyes in Jamaica. Whilst developing a comprehensive disease profile to aid in accurate diagnosis and staging for patients from groups typically underrepresented or not included in research, this study demonstrates a need to further investigate the current state of the disease in Jamaica and expand the clinical characteristics of patients with glaucoma. Additional ongoing work includes medical chart abstraction, evaluation of vision screening findings, and establishing a genetic study of glaucoma in this unique population.
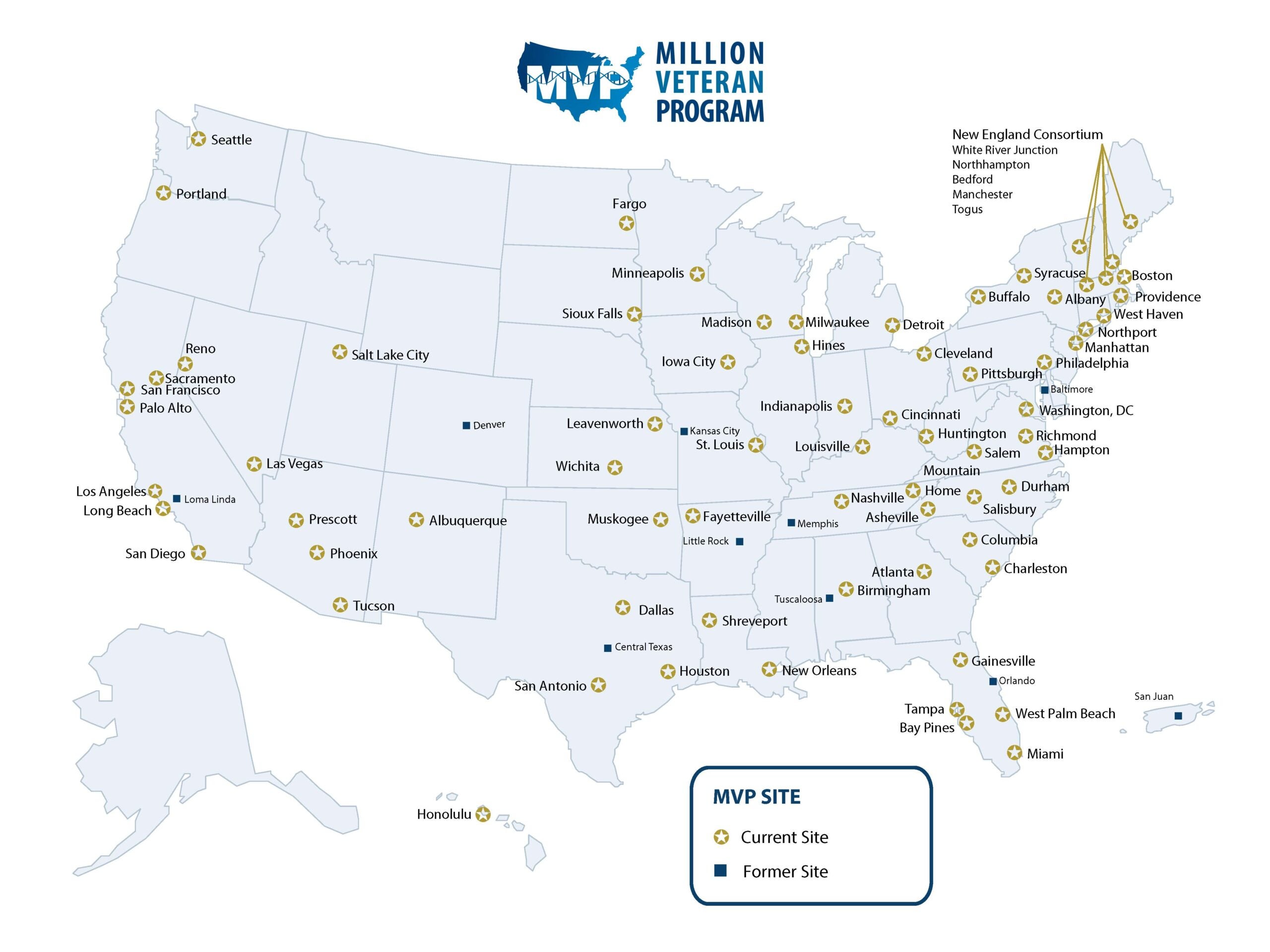
Million Veteran Program (MVP)
ECU Investigator: Dr. Jessica Cooke Bailey
The MVP is a national research program run by the U.S. Department of Veterans Affairs (VA) looking at how genes, lifestyle, military experiences, and exposures affect health and wellness in Veterans. The larger MVP Eye Disease group, led by Dr. Neal Peachey (Cleveland VA) and Dr. Sudha Iyengar (CWRU), studies eye diseases relevant to Veterans. This group also includes Dr. Cooke Bailey’s team, Tyler Kinzy, MS (ECU), Dr. Cari Nealon (Cleveland VA), Dr. Dana Crawford (CWRU), and Lauren Cruz, MPH (CWRU)), conducts research investigating glaucoma genetics, focusing mainly on primary open-angle glaucoma (POAG). Findings from this study include: (i) generated clinician-informed phenotyping algorithms to classify POAG cases and controls (PMID: 34822319); (ii) evaluated a 127-SNP GRS in European-descent and African-descent Veterans and found that, unsurprisingly, it classifies European-descent cases much more accurately than African-descent cases, again to emphasizing the importance of representation of diverse ancestry groups in genetic analyses of POAG (PMID: 35718050); (iii) extending the GRS evaluation to Hispanic Veterans, it performed similarly in Hispanic and European-descent Veterans (PMID: 36540996). Studies underway include leading the largest ever genome-wide meta-analyses of POAG in people of African descent and in Hispanics. Future directions include identifying clinically-relevant variants associated with glaucoma subtypes (normal and high-pressure glaucoma), progression types (individuals that quickly or slowly progress to end-stage glaucoma outcomes), as well as those with poor and adequate treatment responses.
All Eyes on Us
ECU Investigator: Dr. Jessica Cooke Bailey
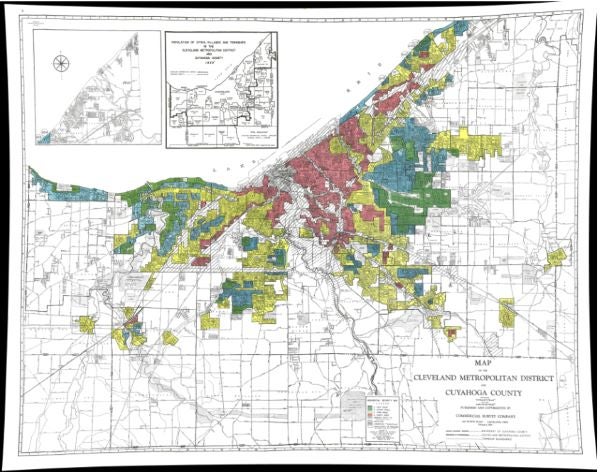
This study was formed in collaboration with Drs. Erika Trapl and Sarah Koopman-Gonzalez, leaders of the CWRU Prevention Research Center for Healthy Neighborhoods, to better understand perceptions, values, and barriers to vision care in a racially and socio-demographically diverse Cleveland, Ohio community. Early diagnosis and intervention are essential for preventing the most severe glaucoma outcomes (severe vision loss and blindness). Our team formed an intentional collaboration with University Settlement, a community resource center with a 92-year history in Broadway-Slavic Village, an interracial neighborhood that is the second poorest in Cleveland. This collaboration built a Community Advisory Board (CAB) to facilitate discussion of vision health and construction of a qualitative interview instrument that would assess perception, values, and barriers to vision health care among Slavic Village neighborhood residents. Participants (60) in this study identified through several channels that accessibility to and awareness about eye health and eye care is an issue in this community.
Trends and Disparities in Mortality in Eastern North Carolina: Total Deaths, Premature Mortality and Deaths for Ten Leading Causes; 1990 – 2021
Principal Investigator (PI): Dr. Katherine Jones
This report provides a visual overview in charts for a 30-year period for the top causes of death for eastern North Carolina in 2021. It includes comparison to other regions of the state as well as comparisons by race and gender within the eastern region. The report is produced every year for a 41-county eastern NC region and a 29-county northeastern region. I am currently preparing the 2021 version for ENC29. This report is prepared with assistance from ECU graduate students. Current assistance is being provided by Ayobami Alimi, a graduate student in the department of Data Science. The 2020 versions were prepared with assistance from Jordan Gaskin, a Masters of Public Health student. Previous year’s versions of the report are available at: Health Indicators
The Trends and Disparities Report is a product of the Department of Public Health.
Disparity in COVID-19 Outcomes for Eastern North Carolina Compared to the State Overall ( 2020 data)
Co-PIs: Dr. Katherine Jones and Dr. Satomi Imai
This recently completed health brief examines differences in COVID-19 mortality rates for the 29-county region of northeastern North Carolina as compared to the state during the first year of the pandemic, with a particular focus on gender and race. Eastern North Carolina has many of the economic and social disparities that were associated with severe COVID-19 in the first year of the pandemic, and the mortality rate was higher in this region than the state for all race and gender groups. This report highlights differences in outcomes, as well as differences in underlying social and health conditions that contributed to those outcomes. Co-Authors: Katherine Jones, Satomi Imai, Aaron Kipp. The brief is available at: Disparity in Covid-19 Outcomes for Eastern North Carolina
Reporting for North Carolina Statewide Telepsychiatry Program (NC-STeP)
Principal Investigator (PI): Dr. Sy Saeed
Key Personnel: Dr. Katherine Jones
The North Carolina Statewide Telepsychiatry Program connects hospital emergency departments and local community sites to provide psychiatric assessments and consultations using telemedicine. The program is funded by the state as well as private foundations and has been in place since 2013, linking hospitals and community clinics across the state of North Carolina with psychiatric services. I have acted as the data and reporting manager for this program and have also participated in various research projects and academic publications based on the program. For more information on the program go to: NC Statewide Telepsychiatry Program
“Maternal Outreach Through Telehealth for Rural Sites: the MOTHeRs Project.” S Saeed, K Jones, A Sacks, K Craven, Y Xue. North Carolina Medical Journal. 2023; 84(1): 45-50.
“The Impact of NC Statewide Telepsychiatry Program (NC-STeP) on Cost Savings by Reducing Unnecessary Psychiatric Hospitalizations During a 6 ½ Year Period.” S Saeed, K Jones, K Muppavarapu. Psychiatric Quarterly. 2021; 93(2).
“The Impact of the North Carolina Statewide Telepsychiatry Program (NC-STeP) on Patients’ Dispositions from Emergency Departments.” R Kothadia, K Jones, S Saeed, M Torres. Psychiatric Services. 2020; (71: 12).
Firearms storage practices in North Carolina homes
Principal Investigator (PI): Dr. Satomi Imai
Key Personnel: Dr. Katherine Jones, Dr. Ann Rafferty, Dr. Huabin Luo, Jordan Gaskin
This study examines demographic, behavioral, and situational factors affecting firearm storage practices in North Carolina homes. The trend, racial/ethnic disparities, and risk factors for suicide while living in households with firearms are further investigated. The findings aim to inform targeted community initiatives promoting safer firearm practices at home, ultimately reducing firearm-related deaths and injuries.
Perceived racial discrimination in healthcare: Healthcare access, health conditions, and race/ethnicity
Principal Investigator (PI): Dr. Satomi Imai
Key Personnel: Sachiyo Shearman, Dr. Katherine Jones, Sandra Garcia Juarez
This study investigates perceived differential racial treatment in healthcare and associated impacts on health. Perceived racial discrimination in healthcare settings adversely affects healthcare access and utilization. Identifying populations vulnerable to such perceptions provides valuable insights to improve communication between patients and healthcare providers.
High school students’ screen time and social-image: Impact on mental health and suicidal ideation
Principal Investigator (PI): Dr. Satomi Imai
Key Personnel: Dr. Katherine Jones, Austin Close
This study examines the adverse effects of excessive use of digital devices on the mental health of adolescents. It explores the connections among social-image variables, depressive thoughts, and suicidal ideation. The findings provide essential insights for educators and parents seeking to identify vulnerable populations that can benefit from targeted interventions.
LGBTQ+ youth victimization and mental health in North Carolina
Principal Investigator (PI): Dr. Satomi Imai
Key Personnel: Jordan Gaskin; Dr. Katherine Jones
This study investigates the impact of victimization on mental health outcomes for LGBTQ+ youth compared to heterosexual youth in North Carolina. The findings reveal that a greater percentage of LGBTQ youth, irrespective of gender or race, experience bullying and suffer from poorer mental health compared to their heterosexual counterparts. These results underscore the need for additional quantitative and qualitative research to explore potential interventions for the most vulnerable individuals.